Depression is a complex medical condition, not a one-size-fits-all diagnosis. For many people, medication plays a critical role in reducing symptoms, restoring daily functioning, and preventing relapse. Psychiatric medication management for depression goes far beyond simply prescribing antidepressants—it is an ongoing, personalized process that prioritizes safety, effectiveness, and the whole person.
This guide explains how medication management works, who provides it, what patients can expect, and how it fits into a comprehensive depression treatment plan.
Understanding Psychiatric Medication Management
Psychiatric medication management refers to the careful selection, prescribing, evaluation, and adjustment of medications used to treat mental health conditions like depression.
Effective psychiatric medication management services focus on:
- Accurate diagnosis
- Evidence-based medication selection
- Regular follow-up and symptom tracking
- Monitoring benefits, risks, and long-term outcomes
The goal is not just symptom relief, but sustainable mental wellness with minimal side effects.
Who Provides Medication Management for Depression?
A qualified psychiatric medication management provider may include:
- Psychiatrists (MD or DO)
- Psychiatric nurse practitioners (PMHNPs)
- Physician assistants with psychiatric training
A medication management psychiatrist is uniquely trained to understand how brain chemistry, physical health, and life circumstances interact—making them especially valuable for complex or treatment-resistant depression.
The Medication Management Process: Step by Step
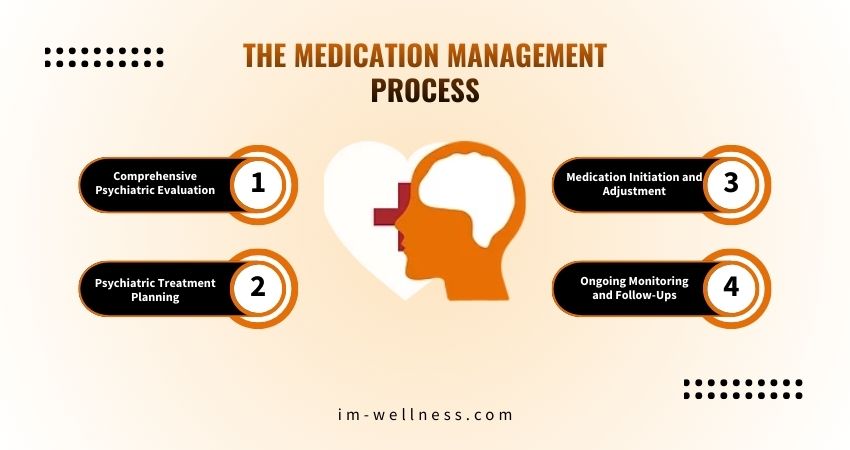
1. Comprehensive Psychiatric Evaluation
Before prescribing, clinicians assess:
- Depression severity and symptom patterns
- Medical history and current medications
- Family mental health history
- Lifestyle factors (sleep, stress, substance use)
This ensures treatment is safe, appropriate, and individualized.
2. Psychiatric Treatment Planning
Effective care includes structured psychiatric treatment planning, which outlines:
- Medication options and rationale
- Expected benefits and timelines
- Possible alternatives if first-line treatment fails
- Integration with therapy or lifestyle interventions
This collaborative approach helps patients make informed decisions.
3. Medication Initiation and Adjustment
Antidepressants may include:
- SSRIs
- SNRIs
- Atypical antidepressants
- Mood stabilizers or adjunct medications (when indicated)
Doses are adjusted gradually based on response and tolerance.
4. Ongoing Monitoring and Follow-Ups
Consistent psychiatric medication monitoring is essential, especially in the first weeks of treatment. Follow-ups help clinicians:
- Track symptom improvement
- Identify side effects early
- Adjust dosages safely
- Prevent relapse or discontinuation issues
Managing Side Effects Safely
All medications carry potential risks. Understanding and managing psychiatric medication side effects is a core part of responsible care.
Common side effects may include:
- Gastrointestinal discomfort
- Sleep changes
- Weight fluctuations
- Sexual side effects
- Emotional blunting
Regular check-ins allow providers to minimize discomfort while maintaining therapeutic benefit.
Medication as Part of Whole-Person Care
Medication is most effective when combined with:
- Psychotherapy (CBT, IPT, or psychodynamic therapy)
- Healthy sleep and nutrition habits
- Stress management strategies
- Social support systems
Thoughtful mental health prescription management ensures medications support—not replace—broader recovery efforts.
When Medication Management Is Especially Important
Medication management is particularly valuable for individuals who:
- Have moderate to severe depression
- Experience recurrent depressive episodes
- Have not improved with therapy alone
- Manage co-occurring anxiety, bipolar disorder, or medical conditions
- Need long-term maintenance treatment
FAQs:
What is psychiatric medication management for depression?
It is an ongoing medical process involving prescribing, monitoring, and adjusting medications to safely and effectively treat depressive disorders.
How long does it take for antidepressants to work?
Most antidepressants show noticeable improvement within 4–6 weeks, though some symptoms may improve earlier.
Do I need medication if I’m already in therapy?
Not always, but for moderate to severe depression, combining therapy with medication often leads to better outcomes.
How often are follow-up appointments needed?
Initially, follow-ups may occur every 2–4 weeks, then less frequently once symptoms stabilize.
Can medication be stopped once I feel better?
Stopping medication should always be done gradually under medical supervision to reduce relapse and withdrawal risks.
Key Takeaways
Psychiatric medication management for depression is a structured, evidence-based approach that prioritizes safety, personalization, and long-term mental health. When guided by a qualified provider and combined with therapy and lifestyle support, medication can be a powerful tool in recovery—not a standalone solution.
You don’t have to navigate depression alone. Compassionate, expert psychiatric care can make a real difference in how you feel and function day to day. At Insight Mental Wellness, personalized medication management is designed to support your mental health goals with safety, clarity, and ongoing care.